From http://epaper.mypaper.sg/emnd/fvxen/fvxp/fvxpress.php?param=2015-01-14
Source Website: http://mypaper.sg/opinion/us-needs-re-look-treating-diabetes-patients-20150114
By Kasia Lipska, NYT, mypaper, myp@sph.com.sg, Published on Jan 14, 2015
FILE PHOTO: THE NEW PAPER
https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEjkxzg8NAzSyccltp4Iyn55UXaxMpNiMlwe3F-hcuzmu20hY_u9p-sFSmpRWO1n-V-ByFQZUVIxaQ70rXqzbfu40x3rSXkUH25gloWVy3WA4QSWBVZfVaMtefWTz1w1hrJawb45_LMR7eY/s1600/US+needs+re-look+on+treating+diabetes+patients.jpg
My Paper, Wednesday, January 14, 2015, Page A7, Opinion
ONE of my elderly patients has type 2 diabetes and heart disease. He takes a number of medications, including insulin to control his blood sugar levels. A few years ago, he was driving when his blood sugar levels suddenly dropped. He felt lightheaded for a moment, and then ran into a tree.
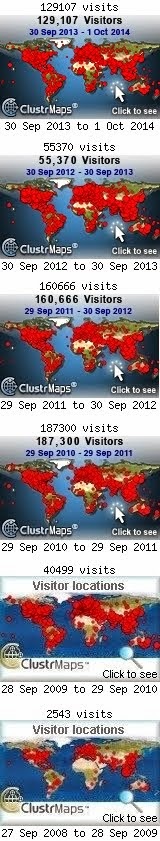
There are roughly 11 million Americans over age 65 with diabetes. Most of them take medications to reduce their blood sugar levels. The majority reach an average blood sugar target, or "haemoglobin A1C", of less than 7 per cent. Why? Early studies showed that this can reduce the risk of diabetes complications, including eye, kidney and nerve problems.
As a result, for more than a decade, medical societies, pharmaceutical companies and diabetes groups have campaigned with a simple message - to get below seven. Many patients carry report cards with their scores to appointments. Doctors are often rewarded based on how many of their patients hit the target.
All of this sounds great. But, at least for older people, there are serious problems with the below-seven paradigm.
The health benefits of this strategy are uncertain for older people. Those early studies were conducted on people with type 1 diabetes or with younger patients with newly diagnosed type 2 diabetes. Subsequent trials of older patients raised doubts about the benefits.
Worse, targeting low blood sugar levels can cause harm. In one instance, investigators actually had to stop a trial early, because patients who were targeting haemoglobin A1C levels of six or below had significantly higher rates of death than patients targeting levels in the sevens.
We don't know exactly why this happened. What we do know is that aiming for levels below seven increases the risk for hypoglycemia, or low blood sugar reactions. Severe reactions can result in confusion, coma, falls, fractures, abnormal heart rhythms and even death.
Older people are especially susceptible to severe hypoglycemia. With age, kidneys become less efficient, which causes insulin (or other drugs) to accumulate in the body; this, in turn, can lead to hypoglycemia.
What's more, older people often take multiple medications, some of which may interact with diabetes drugs. This, too, may cause hypoglycemia. Using multiple medications or complex insulin regimens also increases the chances of errors.
Finally, older people have fewer warning symptoms when they experience mild dips in blood sugar, and this leaves less time for them to treat the problem before it becomes severe. This is what happened to my patient.
Given the questionable benefits and real risks of going below seven, the American Geriatrics Society and the Veterans Affairs diabetes guidelines have, for years, recommended a cautious, case-by-case approach for older patients.
For those with serious health problems or prior history of hypoglycemia, going below seven may not be worth the risks involved. The problem is that we haven't put these guidelines into practice.
In a new study published on Monday in Jama Internal Medicine, my colleagues and I used nationally representative data from 2001 to 2010 and showed that 62 per cent of adults over age 65 went below seven. But here's the catch. We found no difference in how people were treated based on their health.
Patients in poor health and at risk of hypoglycemia tended to be treated as aggressively as far healthier patients. This seems to confirm that we have been adhering to a one-size-fits-all approach, despite the risks that it poses to millions of older Americans.
Part of the problem is that there are strong incentives in place to keep the status quo. The diabetes drug industry has a vested interest in selling its products to as many Americans as it can, and has been incredibly successful at doing so. Sales of diabetes drugs in 2013 were about equal to the combined revenue of the National Football League, Major League Baseball and the National Basketball Association.
There is nothing wrong with the industry selling its drugs, but it is the job of the medical profession to guide what treatment patients receive. To do this properly, doctors with financial ties to the diabetes drug industry shouldn't be writing guidelines on how to use these drugs. At present, this is still common.
Ultimately, changing current paradigms requires doctors to partner their patients in making decisions about treatment. Patients need to understand that there are different options, with different risks. The goal is not to get a perfect score on a report card, but to weigh these risks to make a good decision.
My patient was terrified at the prospect of having another car wreck - a completely reasonable concern - and we decided to use less insulin and let his sugars run higher, in the eights. It's possible that this slightly raises his risk of kidney or eye problems, but this was a risk he was more than happy to take.
By Kasia Lipska, NYT, mypaper, myp@sph.com.sg, Published on Jan 14, 2015
The writer is an endocrinologist at the Yale School of Medicine and a clinical investigator at the Yale-New Haven Hospital Centre for Outcomes Research and Evaluation.
Reference
- My Paper, Wednesday, January 14, 2015, Page A7, Opinion
- http://epaper.mypaper.sg/emnd/fvxen/fvxp/fvxpress.php?param=2015-01-14
- http://mypaper.sg/opinion/us-needs-re-look-treating-diabetes-patients-20150114
- https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEjkxzg8NAzSyccltp4Iyn55UXaxMpNiMlwe3F-hcuzmu20hY_u9p-sFSmpRWO1n-V-ByFQZUVIxaQ70rXqzbfu40x3rSXkUH25gloWVy3WA4QSWBVZfVaMtefWTz1w1hrJawb45_LMR7eY/s1600/US+needs+re-look+on+treating+diabetes+patients.jpg
- My Paper, Wednesday, January 14, 2015, Page A7, Opinion































.jpg)
.gif)
.jpg)